Where HAVE our GPs gone? Shock new figures show just one doctor for every 2,200 patients as NHS staff shortages start to bite… and even routine appointments are axed by more than a third of practices
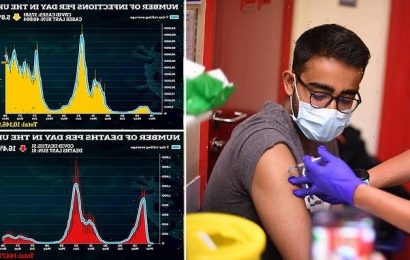
- The are 1,343 fewer GPs now than in 2017, while patient numbers have risen
- Each GP is responsible to care for 2,200 patients because of lack of staff
- Figures show that GPs rush through 20% of appointments in five minutes or less
GPs are being forced to care for 2,200 patients each because of NHS staff shortages.
An extra 3.1million patients have been registered since June 2017 yet the number of fully qualified family doctors has fallen by 1,343 over the same period.
It means each GP has 10 per cent more names on their lists than five years ago.
And a postcode lottery is leaving some areas desperately short of cover, with just one doctor to look after 3,000 patients.
The shocking figures come after NHS Digital revealed that GPs are rushing through a fifth of appointments in five minutes or less.
New figures have revealed that a single GP is responsible for the care of 2,200 people, as patient numbers have risen but the number of family doctors has fallen (stock image)
Daisy Cooper MP (pictured), Lib Dem health spokesman, believes the health system is at a breaking point and that a plan is needed to recruit more doctors
The revelations will pile pressure on ministers to honour their promise of hiring an extra 6,000 family doctors by 2024.
‘The national shortage of GPs means it is a struggle securing an appointment,’ said Dennis Reed of Silver Voices, which campaigns for elderly people. ‘Some people give up trying, which leaves them at risk of deteriorating, while others will end up at the door of busy A&Es. More needs to be done to get doctors into general practice and to stop experienced ones from retiring early.
‘But we need to increase GP numbers equitably, so we can end this postcode lottery of care.’
There were 58.4million patients registered with a GP in England in June 2017, rising 5.4 per cent to 61.57million by March this year.
Meanwhile, the number of full-time and fully qualified GPs fell 4.6 per cent from 29,112 to 27,769 over the same period. It means the number of patients per GP rose by 10.46 per cent, from 2,007 to 2,217.
Blackburn with Darwen was worst off, with 3,004 patients per qualified GP in March, according to analysis of NHS data by the Liberal Democrats.
By contrast, Wirral had just 1,762 patients per GP – the lowest ratio.
Even routine appointments axed by over a third of GPs
More than a third of GP practices have stopped booking routine appointments after being overwhelmed with calls, a survey reveals.
Family doctors say severe staff shortages and unprecedented demand have forced them to turn sick patients away. Of 824 doctors surveyed by GP magazine Pulse, 35 per cent said their surgery had stopped booking routine consultations at some point over the past year.
Dr Nick Morton, a GP partner in Norfolk and Waveney, said: ‘We operate a safety valve system so when we are overwhelmed, we stop pretending we have enough resources. Patients are directed to the walk-in centre, local pharmacies or if they perceive it to be an emergency, A&E.’
The system does not apply to some, including ‘the vulnerable and end-of-life patients’, and is not used often.
But it gives practice staff a ‘sense of being able to cope when deluged with demand’, Dr Morton said.
Dr Gaurav Gupta, a GP and chairman of the Kent Local Medical Committee, said it was ‘not surprising’ practices had been unable to provide services.
In March, GPs in England had more than 15million patient consultations – the highest number since records began, according to NHS Digital data.
Daisy Cooper, Lib Dem health spokesman, said: ‘Our health services are at breaking point following the Conservative Government’s broken promise to recruit more GPs.
‘People are struggling to get appointments and GPs are under more pressure than ever. We need a proper plan to recruit the GPs the country desperately needs and prevent so many doctors leaving or retiring early.’
Commenting on the numbers, Healthwatch England, which represents patients, said access to GP services was one of the most common issues raised by the public. It added: ‘Things need to change for the sake of patient care, staff welfare and the sustainability of the wider NHS.’ Dr Kieran Sharrock, deputy chairman of the British Medical Association’s GP committee, said: ‘With fewer doctors to treat more patients, it’s harder to see people in a timely way and GPs share their patients’ frustration with longer waits.
‘Remaining staff are forced to stretch themselves further, risking their own physical and mental health, which then drives them away from the profession, making the problem even worse.
‘We need the Government to listen to and support GPs and their colleagues, and make good on its pledges to boost the GP workforce so that practices can provide the safe, quality care that patients deserve.’
Dr Rachel Ward, of the Rebuild General Practice campaign, described the shortage of GPs as a ‘national emergency’. She added: ‘Years of underfunding, neglect and broken government promises have led to fewer GPs, at a time when there are more patients than ever.
‘GPs want to provide the best quality care for their patients, but the current situation is unsafe.
‘That’s why we’re calling for urgent support to rebuild general practice.’
More than a third of appointments at GP surgeries were still not face to face in March, the NHS Digital figures show. Many switched to video or phone consultations during the pandemic but have not returned to normal levels. Some 81.0 per cent of appointments took place in-person in October 2019, pre-Covid.
This dipped to a low of 46.7 per cent in April 2020 and climbed to a recent high of 64.3 per cent in October 2021 as restrictions were eased. But only 62.0 per cent of the 29.6million appointments conducted this March at GP surgeries were face to face. This total includes appointments at surgeries with nurses, physiotherapists and pharmacists as well as doctors. Government research shows most GPs now work no more than three days a week.
The study commissioned by the Department of Health and Social Care shows a ‘substantial’ fall in hours worked since the pandemic, with just half of family doctors in work on Friday afternoon.
More than a third of appointments at GP surgeries in the UK were still not face to face in March
A spokesman for the department said the number of GPs in England had increased in recent years when considering those still in training.
They added: ‘We are working with the NHS to improve access to GPs, tackle the Covid backlog, and grow the general practice workforce to ensure everyone receives the care they need – including making £520million available to improve access and expand general practice capacity during the pandemic.
‘There were over 1,400 more full-time equivalent doctors working in general practice in March 2022 compared with March 2019, a record-breaking number started training as GPs last year, and we’ve invested £1.5billion until 2025 to create an extra 50million appointments a year.’
A survey earlier this year revealed that patient satisfaction with GP surgeries has plummeted to its lowest ever level.
Fewer than four in ten patients said they happy with the service. The British Social Attitudes survey found the approval rating had almost halved in the pandemic.
Source: Read Full Article